Endometrial hyperplasia is more likely to occur in women with risk factors, including:
- age older than 35
- never having been pregnant
- older age at menopause
- early age when menstruation started
- history of certain conditions, such asdiabetes mellitus, PCOS, gallbladder disease, or thyroid disease:
- obesity
- cigarette smoking
- family history of ovarian, colon, or uterine cancer
Endometrial hyperplasia also occurs after menopause, when ovulation stops and progesterone is no longer made. There may be high levels of estrogen and not enough progesterone in other situations, including when a woman:
- uses medications that act like estrogen, such astamoxifen for cancer treatment
- uses estrogen forhormone therapy and does not use progesterone orprogestin if she still has a uterus
Endometrial Hyperplasia is usually asymptomatic. However, when it manifests clinically, the most common sign is abnormal uterine bleeding, i.e:
- Bleeding during your period that is heavier or lasts longer than usual
- Menstrual cycles that are shorter than 21 days (counting from the first day of the menstrual period to the first day of the next menstrual period)
- Any bleeding after menopause
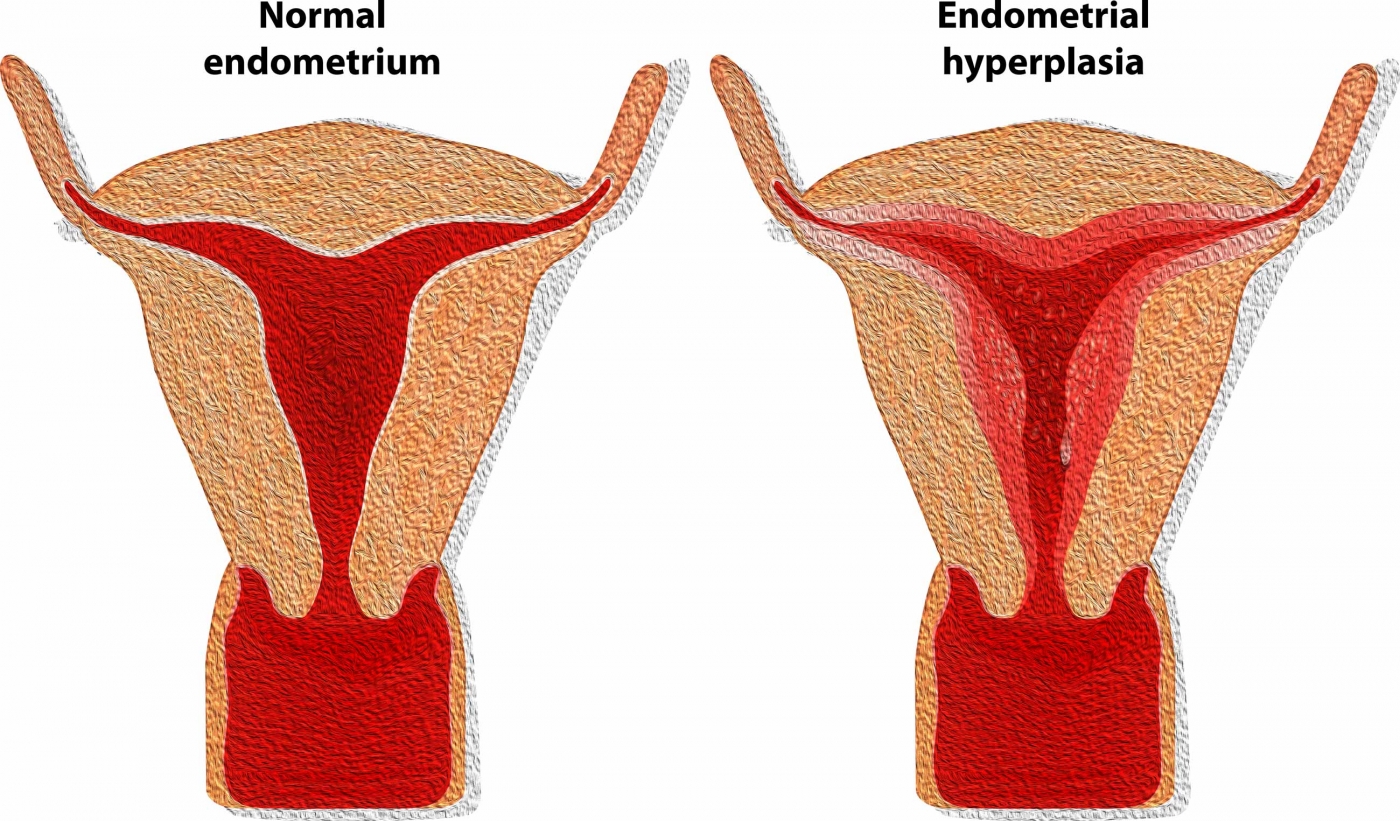
Investigation of the condition is done with a transvaginal ultrasound exam to measure the thickness of the endometrium. However, the only way to confirm diagnosis and to exclude the presence of cancer is to obtain a small sample of tissue from the endometrium for histology. Albeit this was done with an endometrial biopsy during a dilation and curettage (D&C) procedure, hysteroscopy is now the Gold Standard method as it offers direct visualization of the intrauterine cavity and the whole endometrium and the ability to obtain targeted biopsies from suspicious areas.