A thorough preoperative evaluation is imperative because not only benign disease can manifest as abnormal uterine disease. This can include a detailed history, physical examination, ultrasonography and blood tests like full blood count, platelet count, thyroid function and a pregnancy test if applicable.
Endometrial ablation outcomes can be improved by scheduling the procedure immediately after menses. The early proliferative phase (1st half of menstrual cycle) yields better results than operating in the secretory phase (2nd half).
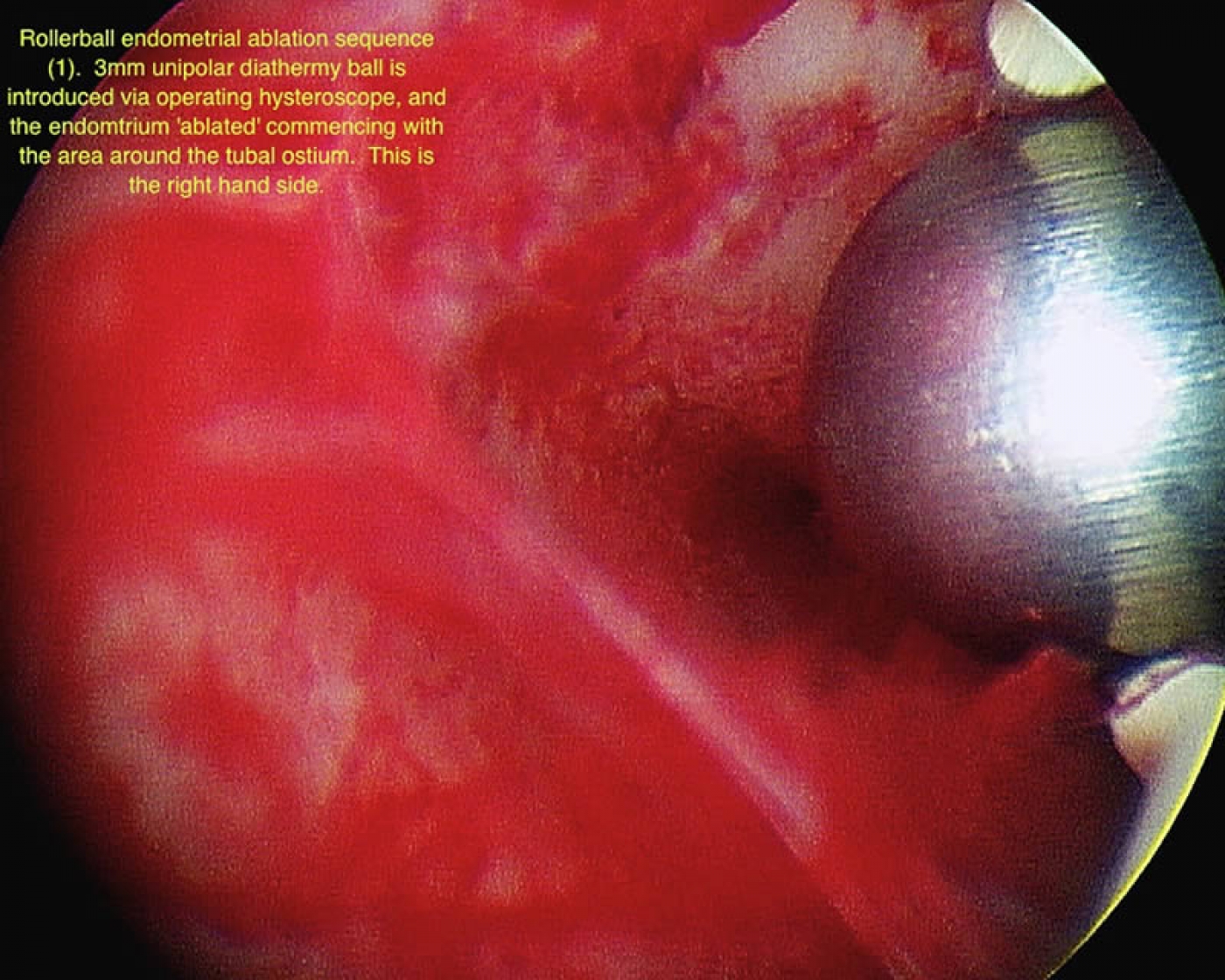
The concept and goals behind endometrial ablation are to create severe endometrial scarification and secondary amenorrhea. The hysteroscope used is called resectoscope through which a variety of operative electrodes can be introduced in the uterine cavity. Thus, the endometrium can be resected in slices (loop electrode) or ablated locally (rollerball electrode). If the latter is chosen, the patient should have an endometrial biopsy performed prior to the hysteroscopic procedure to exclude the possibility of hyperplasia or malignancy.
The majority of patients who undergo endometrial ablation will be satisfied with their clinical outcome as at least 90% of them will have postoperative amenorrhea or notice significant symptomatic improvement. About 5% to 10% of patients may need a repeat ablation procedure or decide to proceed to hysterectomy.